Depression is a mood disorder that affects one in six adults in the UK.
It is characterised by persistently low mood that can last for weeks or months alongside other physical and emotional symptoms. Like many neuropsychiatric disorders, the exact mechanism of depression is not known, and there are many commonly held myths about the disease; three significant ones shall be addressed.
In order to realise modern conceptions of depression, the origins of the disorder throughout history should be understood.
Origins of depression
The first recorded account of depression was from Mesopotamian texts in 200BC. In Ancient Chinese, Egyptian and Mesopotamian societies, and in medieval Europe, depression was thought of as caused by demonic influences. Treatments were often barbaric like exorcism, beatings, starving or imprisonment to stop contagion.
However, there have also been positive understandings throughout history by civilisations like the Ancient Greeks and Romans who recorded it as a disorder. They thought it was caused by grief or a physical imbalance of blood and bile, and had more humane cures of exercise, music, herbal medicine and even marriage.
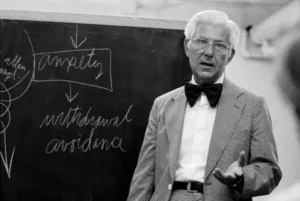
Sigmund Freud fathered the modern understanding of the disorder theorising depression came from repressed shame from early life experiences, which should be worked out through talking therapy (psychotherapy). But it was Aron Beck in the 1960’s who shifted understanding to a more scientific model that’s still used today in diagnoses through the Beck Depression Inventory and in depression talking therapies.
Beck found depressed people suffered from cognitive distortions; negative and hopeless core thoughts and beliefs. He invented the negative triad (pictured right) to show how these thoughts commonly revolved around negative views of (1) the world (2) the self and (3) the future, in his patients studied.
Additionally, their personal explanation of these thoughts are always global ‘it’s just the way I am’, stable ‘I’ve always been that way, it’ll never change’, and internal ‘there must be something wrong with me’. (Abramson, Seligman & Teasdale, 1978).
These beliefs often become inherent in their daily understanding of their lives and for those severely depressed these thoughts aren’t peripheral but predominate their conscious awareness. This can be seen in verbal or non-verbal action. Such as, divided by the triad, refusal to (1) try new hobbies as everything’s boring (2) do daily basic tasks like eat properly as there isn’t any point, or (3) care for future work prospects as they all seem hopeless. This core understanding of depression is still used in diagnostics, Psychotherapy and Cognitive Behavioural Therapy in the NHS and around the world. However, there is more to be unpacked about depression where ‘common knowledge’ has misled people’s understanding.
1. Depression is only in people’s heads
Depression is often assumed to be a low mood that those suffering could pull themselves out of if they had stronger character. This has been proven wrong by scientific developments finding significant physical changes in the brain and body of those with depression. If the physical body is impacted by the disorder, then one can visualise the strength of depression, how it literally isn’t in their heads, and how it can feel so out of their control.
Evidence for these changes is that depression causes changes our immune, cardiovascular and digestive systems. Recent studies from Canada and Germany have also found that physical brain size changes in relation to the disorder. Even further there is evidence that our diets may contribute to depression and that bacteria living in our gut can have a major impact on our mood.
These developments show that depression can’t be oversimplified to a mental state which is easily fixed.
2. Depression is only biologically caused
Studies have shown that the majority of the public believe depression is caused by low serotonin or a chemical imbalance in the brain. However, the British Psychology Society, UCL and a recent overview of all recent evidence show there’s no consistent evidence to support an association between depression and serotonin, the main chemical involved in the supposed chemical imbalance.
Viewing it as a biological disorder may help people understand the significance of depression and promote help between people. However, research has found that believing in this unchangeable scientific origin increases pessimism, therefore limits recovery.
Most recent psychological literature actually states the cause is far more likely significant life events and how people react to them. This in turn may cause the verified physical changes mentioned above. These causal factors range from isolation, unhealthy relationships and grief to marriage and childbirth, and are usually related to a sense of loss of control. This loss of control leads to the self-reinforcing mindset as Beck described, and without others support, it is very difficult for those depressed ‘to pull themselves out’.
There is often confusion around the biological influence on depression as the disorder runs in families; and your chance of developing it is highly influenced by whether relatives have it. But psychologists suggest one inherits an increased vulnerability to have depression, not the disease itself. There hasn’t been a discovered gene for depression, and non-biological factors like children mimicking parents actions or mindsets may play a role in the high hereditary rates.
3. Depression is similar for all people
The final myth which aids our understanding of the disease when disproved is that all depression symptoms are similar. Although the disorder can often be tied together by similar cognitive functions (as Beck showed), depression occurs in vastly different manners in different people. Here are just a few examples of the varied experiences of those suffering.
- ‘Anhedonia’ – inability to feel pleasure or joy in the normal things of life
- Overwhelmed by emotion like sorrow, grief, anger or exhaustion
- Experiencing intrusive thoughts that are distressing and distracting
- Feeling low and exhausted early in the day, for some people this is all day
- Being entirely hopeless about the future.
It’s key to understand the large range of depression symptoms to understand when you or people you know may be suffering from it in order for you to get help, or support others. As it’s not a disease but a complex disorder, caused by many factors, that can be prevented early through gaining back control with aid from others.
What help is available?
If you think you have symptoms of depression, you should see your GP and they may do some basic tests like checking your vitals and doing blood tests, to make sure that there is no other physical cause of your symptoms. Treatment depends on the severity of your symptoms but it can be in the form of either medication or talking therapies.
Anti-depressants are psychiatric medications used to treat depression, with the most common being SSRI’s – serotonin regulators. They are not a cure, but they can help to reduce and control the symptoms of depression. Example of commonly used anti-depressants are Citalopram, Sertraline and Fluoxetine.
Talking therapies include counselling, group therapy and cognitive behavioural therapy (CBT). Depending on the severity of your symptoms, you may be referred to a psychiatrist for more focused treatment.
Is research an option?
At St Pancras Clinical Research (SPCR), we recognise that depression can be a debilitating disease and that it can prevent individuals from functioning in the way that they want. We run clinical trials investigating new medicines for depression disorders such as Major Depressive Disorder, Treatment Resistant Depression, with aim to help improve quality of life for those living with depression.
If you get in touch with us about taking part in research, one of our experienced team will have a confidential phone chat to discuss the study and your suitability based on medical history, diagnosis and current medications. If suitable and you would like to go ahead, we would then invite you for a Patient Information Visit to meet the clinic team, discuss the study in more detail and have the opportunity to ask any questions and raise any concerns you might have.

Useful links
- NHS – depression overview
- Mind UK – mental health charity providing support and helplines
- British Psychological Society – full report of current research
- Healthline – Article on physical impacts of depression
- NHS – Self-help guide
- MadInTheUK – Website showing alternative perspective to the current diagnostic approach to mental healthcare